Obesity And Type 2 Diabetes-How To Overcome it
Wednesday, 18 October 2017
Add Comment
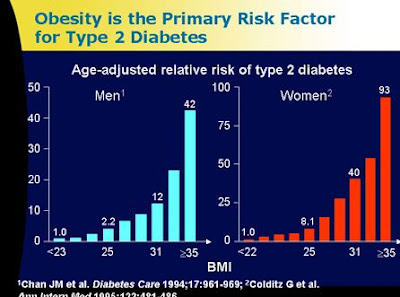
Obesity And Type 2 Diabetes-The prevalence of obesity and type 2 diabetes mellitus
is rising rapidly around the world. About 60% of those who suffer the obes
diabetes mellitus type 2. The greater body mass index (IMT) the greater the
risk of suffering from diabetes mellitus type2.
 |
| obesity and type 2 diabetes |
On the contrary in people with
diabetes mellitus type 2 in the United States ,approximately 90.0% had obes and
power more (overweight). The results of epidemiological studies in developed
countries pointed out that the increasing prevalence of obes in line with the
increasing prevalence of diabetes mellitus type 2.
Wannamethee, dkk2 in the United Kingdom to monitor as
many as 6916 men middle age for 12 years. From the results of monitoring
studies found that the risk of the occurrence of type 2 diabetes mellitus is
increasing significantly and progressively in line with increasing body mass
index and the length is suffering more power or obes(Figure 1).
The results of these epidemiological studies prove that
there is a tight relationship between obesity and diabetes mellitus type 2.
Obesity needs to distinguish between a central or visceral obesity and obesity
peripheral. From the results of epidemiological studies proved that the
Association of obesity and type 2 diabetes mellitus is more apparent in those
with obesity. Inspection results with CT-scan of abdominal visceral fat showed
that contribute towards the onset of insulin resistance. Although fat is a
major Predictor of visceral onset insulin resistance, it seems the relationship
not found in those who are normal weight.
Therefore, it can be inferred that the relationship of
visceral fat and insulin resistance occurs only on the circumstances in which
such excessive visceral fat tissue in people with obes. This article will
discuss about the pathophysiology of the onset of type 2 diabetes mellitus in
obesity and management
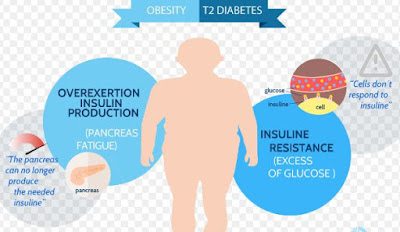
The RELATIONSHIP of OBESITY and type 2 DIABETES MELLITUS
 |
| obesity and type 2 diabetes |
Diabetes mellitus type 2 occurs by two main disorders ,namely
pancreatic beta cellsseptal so that the release of insulin is reduced, and the
presence of insulin resistance. In General, most experts agree that diabetes
mellitus type 2 begins with the presence of insulin resistance, then the
following reduced release of insulin. In people with obes also found the
presence of insulin resistance.
There are allegations that sufferers of
diabetes mellitus type 2 starts with a normal body weight, then becoming obes
with insulin resistance and ended up with diabetes mellitus type 2. In General,
sufferers of diabetes mellitus with typical complaints that come to the clinic
have already found good insulin resistance as well as pancreatic beta cells
septal.
Fatty tissue has two functions as storage of fat in the
form of triglycerides, and as an organ of the endocrine. Fat cells produce a variety
of hormones, also called adipositokin (adipokine) leptin, tumor necrosis factor
alpha (TNF-alpha), interleukin-6 (IL-6), Resistin, and adiponektin. These
hormones also play a role in the onset of insulin resistance. In Figure 2 shown the relationship of fatty tissue with
insulin resistance
The role of free fatty acids
On those who are obese or type 2 diabetes mellitus have
always found the levels of free fatty acids. Increased free fatty acids on
their fat and diabetes mellitus type 2 is caused by increasing the breakdown of
triglycerides (the process of lipolysis) in fatty tissues especially in
visceral. Increasing lipolysis allegedly associated with increased activity of
sympathetic dystrophy of the nervous system. Visceral fat is known as sensitive
to stimulation of nerves sympathetic dystrophy so visceral fat cell metabolism
is very active. High free fatty acids in plasma were cast against the onset of
insulin resistance both on the muscles, liver, and pancreas (Figure 2).
Muscle
In the year 1963 Randle posited the theory that in
circumstances where the increaseof free fatty acids in the blood will be
followed by increasing free fatty acid ambilanby muscle tissue. In normal
circumstances the muscle will use glucose (glucose oxidation) to produce
energy. Thus the oxidation of fatty acids in muscle is increased, this will
inhibit the glucose by muscle ambilan so there was hiperglikemi (Figure 3A).
Hearts
The same situation occurs in the liver, where the heart
will accommodate most of the free fatty acids and become material for the
process of gluconeogenesis and VLDLsynthesis. With increased gluconeogenesis,
fasting plasma glucose is increased then there was hiperglikemi. State of
hiperglikemi this fast will result in insulin resistancein the liver (Figure
3B)
The pancreas
The mechanism of the "damage" the pancreas on
obesity is unclear. It is thought that high free fatty acids will result in the
occurrence of excessive trigliserid deposit onthe pancreas, and the beta cells
will lead to the occurrence of the damage to the beta cells of the pancreas.
A. Combustion free fatty acids increases the amount of
Acetyl CoA, Acetyl CoA overload will hamper the enzyme heksokinase which is an
enzyme important to change the oxidation of glucose into glucose-6-phosphate
(G-6-P). To improve ambilan glucose, muscle cells need more insulin so glucose
can enter into muscle cells, or in other words will occur insulin resistance
B. increased levels of fatty acids in plasma causes the
distribution through the portal system to the liver overload so that more fatty
acids are oxidized and produce Acetyl CoA. Acetyl CoA to activate the enzyme
pyruvate in the liver karboksilase which acts to change glucose into pyruvic
acid on the process of gluconeogenesis, thereby finally happening increased
production and release of glucose liver. Increased gluconeogenesis work
barriers resulted in the liver, insulin or insulin resistance arises.
The role of adipositokin
A recent study proves that adipositokin (adipokin),
which is produced by fat cells play a role in various metabolic processes and
the onset of insulin resistance. Leptin, tumor necrosis factor-alpha
(TNF-alpha), interleukin-6 (IL-6), and improve work resistin resistesi insulin,
rather adiponektin work improves insulin sensitivity.
Leptin
Leptin levels in plasma increases with increasing body
weight. Leptin works at the Central and peripheral nervous system. The role of
leptin against the onset of insulin resistance is unclear. Research on rats,
leptin inhibits phosphorylation of insulin receptor substrate-1 (IRS) which
consequently impedes ambilan glucose. In contrast, other studies in animals
with diabetes obes and leptin, delivery increase insulin sensitivity. Similar
things are also reported human studies.
Tumor necrosis factor-alpha
Same with leptin and free fatty acid, plasma TNF-alpha
levels increased with increasing weight, and plays a role in the mechanism of
peripheral insulin resistance. However, on human levels of TNF-alpha in
circulation very little to inhibit insulin work on muscle tissue. Alleged work
of TNF-alpha more parakrin than the endocrine, or by other factors, such as
free fatty acids, as TNF-alpha stimulate lipolysis. Adipose tissue in rats and
humans, TNF-alpha is expressed in excess so that interfere with insulin
signaling in the phosphorylation of IRS-1 consequently hampered and suppress
the expression of glucose transporter (GLUT)-4.
Interleukin-6
As a proinflamasi protein secreted by adipose tissue,
IL-6 also increased with increasing body weight. In humans, the IL-6 spur the release of glucagon and cortisol and increases
gluconeogenesis. Bastard, et al. found that sufferers of diabetes mellitus that
obes are more resistant to insulin, the levels of IL-6, TNF-alpha and leptin
increased compared to controls not the diabetes mellitus sufferer obes. The
role of IL-6 on insulin resistance is suspected through (adiposity), are not
directly related to the work of insulin. It is reported by Vozarova, et al.
which found that the levels of IL-6 have a correlation with body fat percentage,
but there is no correlation with insulin sensitivity at the Pima Indians.
Resistin
Lazar, et al found a signalling molecule secreted by
the deposit and was named resistin. Increased levels of resistin in mice obes
induced obes and overeating due to genetics, and reduced by administering anti
diabetic drugs agonis peroxisome proliferator-activator receptor (PPAR), such
as rosiglitazone.
Adiponektin
Adiponektin peptide hormones are mainly generated by
adiposit. Compared with other adipositokin, adiponektin the highest levels in
circulation. Adiponektin has an effect contrary to the other adipositokin,
namely, preventing the onset of insulin resistance and diabetes mellitus type
2. Weyer et al, reported levels of adiponektin on white people and Indians Pima
decreases. Adiponektin levels also correlated with insulin sensitivity, and
conversely diminished by increasingly poor glucose tolerance. Other studies in
humans, levels of adiponektin increases with the weight loss and the granting
of agonis PPAR, rosiglitazone. Work adiponektin allegedly with spur expression
genes that regulate the metabolism of fat in the muscle tissue, i.e., CD36,
acyl co-enzyme A (CoA) oxidase, and uncoupling protein (UCP)-2 which will
improve the efficiency of the transport of fatty acids, and fat burning
termogenesis.
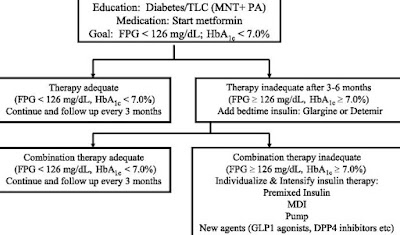
MANAGEMENT
 |
| obesity and type 2 diabetes |
Management on every sufferer of diabetes mellitus
treatment consist of a non-medical nutrition therapy i.e. Pharmacology term
(planning to eat), sports, education, and the use of drugs to lower blood
glucose levels. Specifically for sufferers of type 2diabetes mellitus in
non-obese treatment Pharmacology term is very important, because of the weight
reduction can only be achieved with medical nutrition therapy and improve body
activity/sport. It has been proven that with increasing weight > 10% of
initial weight will increase the risk of diabetes mellitus. In contrast with
the weight loss diabetics mellitus fat can improve the situation of glucose
intolerance.
Management non-Pharmacology term
Non treatment Pharmacology term indeed became the main
goal of diabetes mellitus in obese, non-therapeutic Pharmacology term
unfortunately it doesn't always work, even more often fail. Therefore, some
efforts have sought to keep trying to lose weight sufferers of diabetes
mellitus type 2 are obese, with the addition of the antiobesity drugs such as
orlistat and sibutramin. Because diabetics mellitus fat is often accompanied by
a variety of other metabolic disorders like insulin resistance/hiperinsulinemi,
high levels of cholesterol-low accompanied trigliserid HDL and hypertension, by
itself treatment in diabetics mellitus fat must be taken into account all of these
factors (Figure 4)
Management farmokologik
Oral hypoglycemic drugs
On a currently marketed as much as five types of oral
hypoglycemic drugs, namely sulfonilurea, non-sulfonilurea secretogogue
(repaglinid, natiglinid), biguanid, alpha glucosidase inhibitors (akarbose),
and thiazolidinedion (pioglitazon, rosiglitazon). Oral hypoglycemic drugs in
the election for diabetes mellitus type 2 fat always to be aware of the side
effect of increasing the levels of plasma insulin, and increasing weight. The
thiazolidinedion, metformin, akarbose and repaglinid are recommended for obese
type 2 diabetes mellitus. In certain circumstances the combination treatment
needs to be done in addition to single lowers Metformin blood glucose levels
also lose weight, therefore it is highly recommended in people with diabetes
mellitus type2 fat.
The thiazolidinedion is very good for sufferers of diabetes
mellitus type 2 are obese due to improve insulin sensitivity in the network,
but can sometimes raise the weight. At the moment it has marketed the drug
combination in a single tablet likeGlucovance (metformin-glibenklamid) and
Avandamet (metformin – rosiglitazon). Both of these drugs give good results in people with diabetes mellitus
type 2 are obese, by not raising the weight
Medications associated with cardiovascular risk factors
Because of the prevalence of hypertension, dislipidemi
is very high in people with diabetes mellitus, while targets to be achieved
very tight then drugs related to cardiovascular risk factors such as drug
antihipertensi, hipolipidemik almost routinely given.For the drug
antihipertensi for levels of creatinin in normal limits, the first choice is
the ACE-inhibitors. Specially when it's been discovered the existence of
mikroalbuminuri then the ACE-inhibitors can prevent diabetic nephropathy
perlangsungan worse. The Statins to date is still the first choice for diabetic
dislipidemi in people with diabetes mellitus type 2, except in those with high
levels of trigliserid i.e. > 400 mg/dlthen the fibrat precedence.
The research of the Heart Protection Study using
simvastatin 40 mg/day concluded that those with LDL-cholesterol levels < 100
mg/dl may still provide benefits prevention of cardiovascular complications.
The American Diabetes Association recommends administering aspirin routinely in
people with type 2 diabetes mellitus who > 30 years. It can therefore be
concluded that the majority of sufferers of diabetes mellitus type 2 will
receive preventative medicine for cardiovascular events.
Anti obesity drug
Anti obesity drugs such as orlistat and sibutramin,
greatly help to lose weight in fat sufferers. The medications in addition to
providing weight reduction, it can also provide repair serum lipid profile such
as lowering LDL-cholesterol levels and triglycerides, and raise HDL-cholesterol
levels. Excellent results in weight can be lowered by 10%of initial weight.
Read also:Type 2 Diabetes Symptoms, Causes, And Treatment
Read also:Type 2 Diabetes Symptoms, Causes, And Treatment

0 Response to "Obesity And Type 2 Diabetes-How To Overcome it"
Post a Comment